What does it mean for the cervix to get cancer?
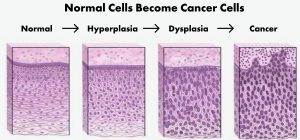
Every woman has a cervix with a thin tissue layer covering it. This tissue comprises many healthy cells that grow and split up before new ones replace them. However, when you develop cervical cancer (cancer of the cervix), the once healthy cells are now cancer cells that act abnormally. The cancer cells grow and split faster than the healthy cells, causing the cancer cells to spread to the deepest layers of cells and nearby organs. Once there gets to be too much cancer cell growth in one area, it causes a tumor to form.
Do a lot of people get cervical cancer?
About 12,000 Americans are diagnosed with cervical cancer annually. Sadly, around 4,000 American women die yearly because of cervical cancer.
How fast does cervical cancer develop after the early signs are detected?
The early stages of cervical cancer show signs of abnormal cervical cell growth called dysplasia. But it can take years before the abnormal cell growth becomes cancerous. So, it is best to seek treatment as early as possible.
What is the primary cause of cancer of the cervix?
Getting infected with the human papillomavirus (HPV) is the primary cause of cervical cancer in women. Sexual activity is the number one way HPV is transmitted from one person to another.
Anyone infected with a high-risk HPV strain has a significant chance of developing cancer in several areas. For example, someone could get cancer of the cervix, anus, penis, vulva, vagina, neck, or head from engaging in sexual activity with an infected person.
Does having an HPV infection mean I will get cervical cancer?
Once HPV infects your cervical cells, they will no longer act normally. Fortunately, most women have strong enough immune systems to eradicate the virus before it causes long-term health problems. But if your immune system cannot eliminate the virus after two years of infection, you will have a higher risk of developing cancer.
What is the best way to avoid getting an HPV infection?
The best preventative measure is to receive the HPV vaccine before getting infected with HPV. It is an effective and safe vaccine with a high success rate of preventing high-risk HPV infections. If you can prevent these infections, you can avoid getting cancer or genital warts. It’s also important to build your immune system by sleeping well, having a healthy diet, and talking HPV supplements that are a preventative measure. AHCC has been shown to support healthy immune function.
When is the best time to receive the HPV vaccine?
Most health experts recommend male and female children should get the HPV vaccine at 11 or 12 years old. Receiving the vaccine before entering their sexually active years will ensure they are protected from a potential HPV infection.
Anyone between 11 and 26 should seek out the HPV vaccine immediately if they haven’t gotten it yet. An unvaccinated person between 26 and 45 should talk to their primary care physician about whether the HPV vaccine is right for them.
Who has the highest risk of developing cervical cancer?
Cervical cancer can occur in women of any age. However, in most cases, women over 40 have a higher risk of developing cervical cancer because they have longer sexual histories and weaker immune systems.
Overall, the HPV type is the most significant factor in whether you could get cervical cancer. High-risk HPV types, such as HPV-16 and HPV-18, cause more cases of cervical cancer than any other HPV type.
Some of the other factors associated with cervical cancer include the following:
- Having sex with numerous partners
- Having sex with a promiscuous man with a vast history of sexual activity
- Having sex when you’re younger than 18
- You smoke tobacco products
- Your family has a history of getting cervical cancer
- You have a medical history of getting dysplasia of the vulva, cervix, and vagina
- You have chlamydia or another sexually transmitted infection
- You have immunodeficiency issues (immune system problems)
- The drug “diethylstilbestrol” was given to your mother when she was pregnant with you
Can I get screened for cervical cancer?
Yes. Your doctor can give you a pap smear (pap test) to check for signs of abnormal cervical cell growth. They may also want to provide you with an HPV test to check for signs of a high-risk HPV infection.It is best to receive regular pap smears before noticing any signs of HPV infections or abnormal cell changes. The earlier these signs are detected, the better your chance of avoiding cancer by receiving treatment before cancer cells develop.
What are the typical cervical cancer symptoms?
No symptoms are usually present in the early stages of cervical cancer and dysplasia. But once the cancer cells grow and spread too much, you will experience symptoms like vaginal bleeding, water discharges, and spotting. In fact, your menstrual bleeding will likely be more excessive than usual. You may even bleed more during sex too.
Many people with cervical cancer may experience symptoms because of other health issues they have as well. However, you won’t know until you visit your primary care physician for a physical examination and lab testing. Based on the results, your doctor can prescribe and administer the necessary treatment to eliminate other health problems and reduce the symptoms as much as possible.
Advanced stages of cancer bring even more severe symptoms, such as urination difficulties, leg swelling, and pelvic pain. These symptoms usually occur when the cancer cells spread beyond the cervix and move toward other organs next to it.
For instance, you may have a cancerous tumor grow so big that it puts pressure on the bladder and causes pain and urination problems. Sometimes a tumor can grow into a vein and restrict the blood flowing through it. In any of these situations, seeking professional medical treatment is the only thing you can do.
How does a doctor diagnose cervical cancer?
First, your primary care physician will perform a pap smear to look for signs of cervical cancer. If any signs are detected, the next step is to perform a biopsy to verify the cancer. Then you will receive the official cervical cancer diagnosis.
From that point forward, the primary care physician will study how much the cancer cells have spread and their potential risks to nearby organs. Your doctor will perform tests like the following:
- Pelvic Examination – The doctor will inspect all the essential organs close to the cervix, such as the uterus and ovaries.
- Cystoscopy – The doctor uses a lighted device to inspect the inside of the bladder and urethra.
- Colonoscopy – The doctor uses a narrow colonoscope device to examine the colon.
Your doctor may recommend additional testing if they believe the cervical cancer cells have spread beyond the cervix to nearby organs.
What does the term “staging” mean?
Staging refers to the cancer stage or how far the cancer cells have spread or progressed. Most doctors use four stages (Stage 1 to Stage 4) to judge the level of cancer progression, although cervical cancer also has an additional stage (Stage 0 to Stage 4).
The lowest stage number represents the least cancer progression, while the highest means the most cancer progression. So if you have Stage 0 cervical cancer, cancer cells are detected on the upper cervical layer only. But if you have Stage 4 cervical cancer, the cancer cells have spread to the deepest cervical tissue layers and onto other nearby organs.
Stage 0 is the noninvasive cervical cancer stage, whereas Stages 1 through 4 are the invasive cancer stages. Let’s explore each invasive cancer stage to understand them better:
- Stage 1 – The cancer cells exist on the cervix only. Additional substages of Stage 1 exist that are worth noting below.
- Stage 1A – The cancer cells have spread a couple of millimeters into the cervix’s deepest layers
- Stage 1B – The cancer cells have spread more than a couple of millimeters into the cervix’s deepest layers
- Stage 2 – The cervical cancer cells have begun to spread to the pelvis and vaginal regions
- Stage 3 – The cervical cancer cells have spread further into the pelvis and vaginal regions
- Stage 4 – The cervical cancer cells have spread to nearby organs, including the rectum or bladder.
Doctors often break down the other stages into multiple substages, but you get the idea.
What kinds of treatments are available for cervical cancer?
The doctor will recommend a particular treatment based on the current cancer stage. Several treatments could be recommended if you are in the later cancer stages.
The best cervical cancer treatments at any invasive stage are chemotherapy, radiation therapy, or surgery. But it is better to get the treatments in the earlier stages before the cancer cells spread to other organs in the body.
Stage 1 cancer patients have a 91% survival rate for five years. On the other hand, Stage 4 cancer patients have a 17% survival rate for five years. That is why treatment in Stage 1 is always better.
What happens during a surgical procedure for treating cervical cancer?
When your doctor wants you to get surgery to treat your cervical cancer condition, they will surgically remove the cluster of cancer cells or the tumor that has grown in your cervical region. However, the doctor may want to perform a hysterectomy to remove your uterus and cervix in order to remove the cancer cells along with them. They won’t touch the ovaries if they appear to be in healthy condition. But if the doctor performs a radical hysterectomy, the doctor will remove a tiny portion of the upper vagina and the supporting structures of the uterus. These parts and structures may include lymph nodes, fallopian tubes, and ovaries.
What can I expect from a radiation therapy procedure to treat cervical cancer?
A radiation therapy procedure applies radiation to cancer cells to stop them from growing and spreading. The doctor may use one of two methods for applying the radiation:
1) Apply radiation to the body externally, so it can go through the skin to target the tumor. This method requires you to receive the treatment daily for about 3 to 4 weeks.
2) A device is placed inside the body to directly apply radiation to the tumor. This method is usually an outpatient procedure, but sometimes you may need to visit the hospital.
Please note that radiation therapy may cause unpleasant symptoms, such as vaginal dryness, vaginal narrowness, bowel damage, bladder damage, or ovary damage.
What can I expect from getting chemotherapy to treat my cervical cancer condition?
Doctors administer chemotherapy drugs in an attempt to kill the cancer cells. Sometimes a doctor will have the patient come to their office to receive chemotherapy in cycles, while others may require the patient to stay at the hospital for a larger dosage. In addition, advanced stages of cervical cancer may require radiation therapy alongside chemotherapy drugs to increase the likelihood of success.
Will I need follow-up treatments?
Cervical cancer should not return after the cancer cells have been eliminated. However, we’d still recommend you come for several follow-up appointments and checkups to screen for cervical cancer within the first couple of years following the initial procedure. It is the best way to ensure the cancer cells have not grown back.
Patients who had their cervixes removed should still get screened for cervical cancer. The doctor will take a cell sample from the upper vaginal region to test for cancer.
Glossary
Anus – Bowel movements exit through this digestive tract opening.
Biopsy – A small tissue sample gets taken during a simple surgical procedure. The purpose is to study the tissue in a laboratory more closely.
Bladder – The body stores urine in this muscular but hollow organ.
Cells – Every structure, organ, and part of the human body contains these tiny building blocks of life.
Cervical Intraepithelial Neoplasia – The human papillomavirus (HPV) infects the cervix and causes abnormal cervical cell changes.
Cervix – The upper vagina features this narrow, lower part of the uterus.
Chemotherapy – Drugs administered to treat cancer.
Co-Testing – Cervical cancer screening tests involving an HPV test and a pap smear.
Dysplasia – Noncancerous abnormal cells replace normal cells
Fallopian Tubes – A human egg leaves the ovary and passes through these tubes until it reaches the uterus
Human Papillomavirus (HPV) – A group of similar virus types, some of which are higher-risk virus strains known to cause genital warts and various cancers. These cancers could affect the mouth, throat, anus, penis, vagina, vulva, and cervix.
Hysterectomy – A surgical procedure to take out the uterus from the body; Uterus removal
Immune System – The natural defense system of the human body that eliminates bacterial and viral invaders to prevent disease.
Lymph Nodes – Round and small bean-like tissues that store a special liquid to lubricate and stimulate body cells. The liquid passes through lymph nodes to reach the body cells.
Ovaries – These female reproductive organs produce and store eggs. They are needed for a woman to get pregnant and generate essential hormones, such as testosterone, estrogen, and progesterone.
Pap Smear (Pap Test) – A cervical cancer screening test where the doctor takes a cell sample from the cervix or vagina and studies it under a microscope to look for abnormalities or cancer.
Radiation Therapy – Radiation treatment applied to cancerous cells
Sexually Transmitted Infections – Transmitting an infection during sexual activity. The most common sexually transmitted infections are HPV, gonorrhea, chlamydia, syphilis, human immunodeficiency virus (HIV), and herpes.
Urethra – Urine leaves the body by passing through this tube-like structure.
Uterus – A woman’s pelvis contains this muscular organ to carry and support her fetus.
Vagina – A muscular tube-like structure that connects the outside of the body to the uterus inside the body.
Vulva – The genital area on the outside of the female body.