According to the Centers for Disease Control, the human papillomavirus (HPV) has caused around 91% of the total number of cervical cancer cases.
Roughly 200 different HPV types are in existence, but only around 40 HPV types get transmitted from sexual activity. However, no penetration is necessary for HPV to be transmitted. Instead, there only needs to be intimate skin-to-skin contact of the genitals, throat, mouth, and anus.
Therefore, you can contract HPV from oral sex, anal sex, and traditional vaginal sex. You can even contract HPV from using the same sex toys as an infected person. That is why health experts recommend you wear dental dams and condoms to lower the risk of contracting HPV from sexual activity. Of course, you will not have 100% protection, but at least it can significantly reduce the risk of infection.
Most sexually active people will contact an HPV strain at least once within their lifetime, usually within the first couple of years they have sex. It does not matter if your partner is a man or woman because every sexually active person is susceptible to the virus. So you don’t have to feel bad if you receive an HPV infection diagnosis because most sexually active people will receive the same diagnosis within their lifetimes.
Fortunately, most HPV-infected people will contract a low-risk HPV strain that the immune system eliminates within two years. These people never even realize they have the virus because they never experience any symptoms.
Sadly, the risk of symptoms and cancer rises for the unfortunate few whose immune systems cannot eliminate the virus.
High-Risk HPV Strains
High-risk HPV strains, such as HPV 16 and HPV 18, have the most potential to cause cervical cancer to develop in women. These strains produce abnormal cervical call changes that eventually become cancerous unless detected and treated quickly.
In addition, a person with a high-risk HPV infection could develop anal cancer, penile cancer, throat cancer, vaginal cancer, or vulval cancer. But cervical cancer is usually the type of cancer most concerning to women with HPV.
Symptoms of Cervical Cancer
If you’re a woman who makes regular appointments with her gynecologist, they will screen you for precancerous cervical cells and early-stage cervical cancer. It is critical to make these appointments because catching the early stages of cervical cancer will give you the greatest odds of treating it successfully.
The symptoms of cervical cancer are as follows:
- Small amounts of blood or spotting between or after periods
- Periods that are longer and heavier than normal
- Bleeding following sexual intercourse, a pelvic examination, or cleaning your vagina
- More discharge from your vaginal area than normal
- Pain when having a sexual encounter
- Pain in your hips or back that you cannot figure out or explain
Make an appointment with your physician if you experience any of these symptoms.
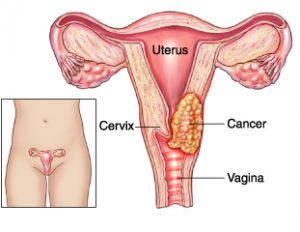
Overview of Cervical Cancer
Cervical cancer is cancer of the cervix in women. When cervical cells undergo abnormal changes from a virus like HPV, they could develop into cervical cancer if left untreated.
Most cervical cancer cases result from high-risk HPV infections. According to the CDC, about 45% of adult males and 40% of adult females contracted HPV between 2011 and 2014. These percentages are less than they were before the HPV vaccine was introduced in 2006. Unfortunately, HPV infections still cause an average of 36,500 HPV-based cervical cancer cases annually.
The good news is that most women with an HPV infection won’t end up with cervical cancer. Only a small percentage of HPV-infected women are diagnosed with cervical cancer. But keep in mind that some women can still get cervical cancer without contracting HPV, but it is extremely rare.
All women need to make at least one visit to a gynecologist per year. It is the most effective way to detect the early stages of cervical cancer. After all, you’ll not likely experience any symptoms during the early stages. Only a licensed gynecologist has the skills to screen you for the early stages of cervical cancer before it develops into something more noticeable and harder to treat.
Make an appointment with your gynecologist and request a pap smear to test for cervical cancer. During the procedure, the doctor will extract a few cervical cells and examine them in a laboratory to see if abnormalities are present. If they are detected, it could be a sign of precancer cells developing. At this point, you still have a good chance of treating the cells before they become cancerous.
The American Cancer Society states that women between 25 and 65 should get an HPV test and pap smear every five years. But if a woman can only get a pap smear and not an HPV test, she should get the pap smear every three years.
In slight contrast, the American College of Obstetricians and Gynecologists believe women between 21 and 29 should get pap smears every three years; and women between 30 and 65 should get pap smears and HPV testing every five years.
However, if you are a woman considered a high cancer risk due to being immunocompromised, your doctor may recommend more frequent testing than the average woman.
Stages of Cervical Cancer
Cervical cancer is identified in the following stages of development:
Stage 1
Cervical tissue has cancer cells spreading deep within it past the surface but not outside the cervix.
Stage 2
The cancer cells grow outside of the cervix as well as the uterus, but they have not gotten to the pelvic walls or lower vagina yet.
Stage 3
Cervical cancer cells grow and make their way to the pelvic walls or lower vagina.
Stage 4
The cancer cells have spread to the rectum, bladder, or any other place far from the cervix, such as the bones and lungs.
Get Medical Care
You must receive consistent medical care from a qualified physician at any of these stages. It is the best way to control and prevent cancer from developing into more advanced stages and symptoms